The goal of the new Transparency in Coverage rules is to make key personalized pricing information easily available to healthcare consumers. These regulations affect non-grandfathered group health plans, individual insurance providers, and non-governmental health plans. They’ll go into effect over the next three years with the following milestones:
- By July 1, 2022: Post machine-readable files outlining in-network rates and out-of-network allowed amounts.
- By January 1, 2023: Provide an internet-based self-service tool that lists personalized, out-of-pocket cost estimates and other price-related data for 500 pre-determined items and services.
- By January 1, 2024: Expand the internet-based tool to include all covered items, services, and prescription drugs in addition to the original 500.
With over 10 years of experience creating innovative solutions to meet the needs of the market and help navigate the complexities of care, Castlight is well-positioned to assist both employer plan sponsors and insurance issuers with rapidly interpreting and responding to these transparency regulations.
Castlight’s Roots
Over the past decade, Castlight has become a leader in healthcare navigation. Our world-class digital platform and team of clinical and benefits experts help members connect with the right care at the right time. Transparency is one of the many factors it takes to empower, engage, and activate someone in their personal healthcare journey.
Fortunately, when it comes to transparency, we’re already at a huge advantage. In the early days of Castlight, we developed deep data expertise in order to equip members with the information needed to make the most informed healthcare decisions. In establishing and mastering the following fundamentals, Castlight became an industry pioneer in transparency.
- Provider Directory: Castlight’s unified provider directory consists of 910,000 physicians. Using our own machine learning model, we regularly validate the accuracy of the provider network information received from multiple sources and claims.
- Cost Estimates: Even before the federal transparency rules were developed, Castlight used an algorithm that combines multiple sources with individual-level data to provide accurate out-of-pocket estimates, 90% of which fall within a 10% error margin.
- Provider Quality: We leverage 30 third-party quality sources — like CMS and IQVIA — and supplement them with Castlight’s proprietary quality score, allowing us to reflect the quality for 94% of physicians and 93% of acute care hospitals in the U.S.
- User Ratings : By adding member ratings and third-party reviews covering around 90% of the unified provider directory, we further enable members to make informed decisions.
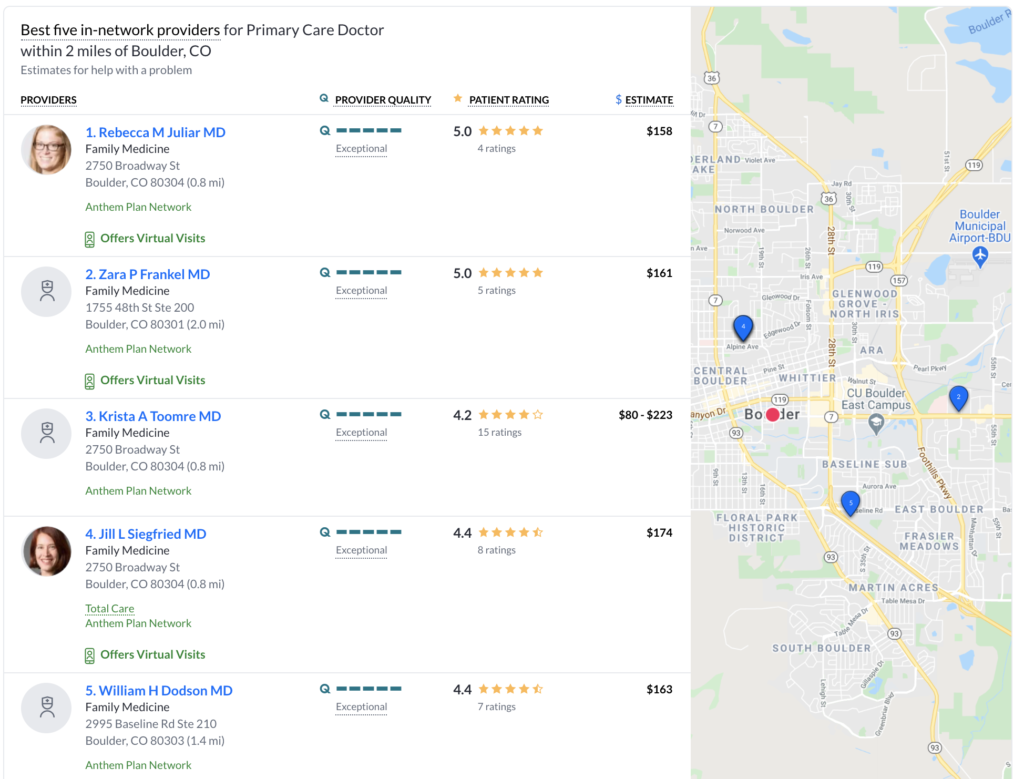
- SmartMatch: Created by Castlight, SmartMatch curates a personalized list of top providers based on cost, quality, convenience, and relevance to a member’s profile and preferences. Members can still search all in-network providers, but SmartMatch gives them a head start, lessens the cognitive burden, and increases engagement.
Castlight’s Transparency in Coverage Solutions
We believe Castlight is prepared for the future of price transparency for three main reasons: We were the first comprehensive transparency solution and have invested significant capital in advancing our capabilities in this space; we have seen it all when it comes to data management and are prepared to accommodate even the most complex pricing data scenarios; we have already built the complementary features that drive personalized engagement and real value in transparency.
Here’s how Castlight’s strong transparency foundation will help plan sponsors and issuers become and remain compliant with these new rules.
Machine Readable Files
Machine Readable Files are a new, important input to the world of price transparency. The files contain rates for specific items and services in each plan. When used in isolation, though, data in the Machine Readable Files does have its limitations.
For example, a Machine Readable File may list a price for a specific item or service rendered by a specific provider, but the files do not contain the contextual information needed to determine if the provider actually provides that item or service. Nor do they contain whether or not the provider is the highest quality, most cost-efficient provider that could render this item or service.
At Castlight, we view Machine Readable Files as one of many valuable inputs that can be stitched together to give individuals all of the right data points they need on price, quality, and convenience to make informed care decisions.
Internet-Based Self-Service Tool
The solution below is Castlight’s current transparency and care guidance experience — when members use Castlight to search for a provider, they see cost estimates, quality scores, and patient ratings. We had this down to a science before the rule came about, and we’ll continue to invest in it as part of our navigation solution.
Today, our platform allows members to search for care by using common language descriptive terms like “asthma” and “dermatologist,” and it also makes sense of items and services typically bundled together in common episodes of care. For example, if someone searches “knee replacement surgery,” they’ll see everything included in the cost estimate.
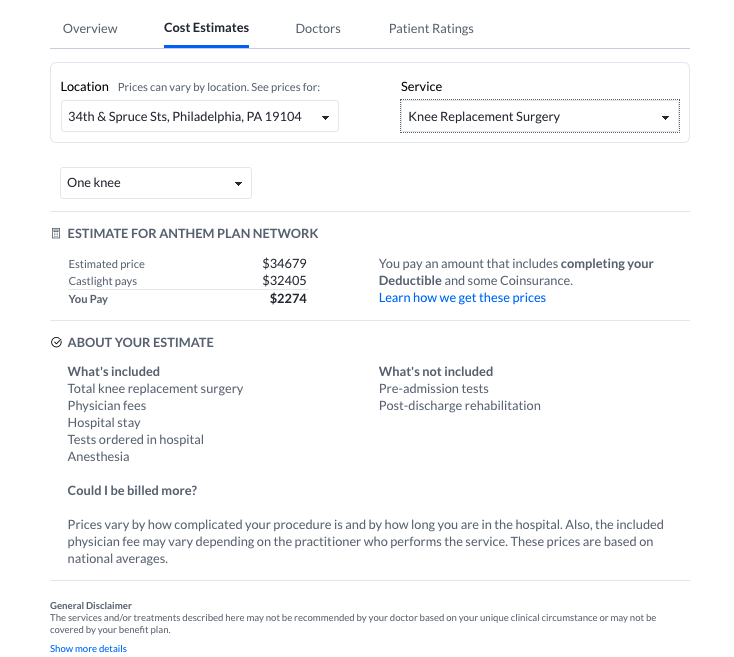
The historical investment made to build this logic already takes cost transparency from a line-item by line-item approach to a more holistic and user-friendly view of cost. The transparency regulations will not cancel out this substantial value. Castlight will continue to view price transparency as one of the many inputs needed to change individual behavior and make informed healthcare decisions.
Looking Forward
We’re excited to help our customers navigate this important evolution in price transparency. However, we want to be clear that we will go far beyond transparency in order to create a healthcare navigation experience consumers actually want to engage with, one that’s personalized to each user and employs several methods to help them find and engage with the best care. We cover that here.
In addition, though it’s completely separate from Transparency in Coverage — and less prescriptive and detailed — the No Surprises Act is equally important. Among other transparency-related provisions, it requires health plans to offer a price comparison tool similar to the internet-based self-service tool required by Transparency in Coverage.
For health plans interested in learning more about how Castlight can help address Transparency in Coverage, visit castlighthealth.com/health-plans/. For self-insured employers, reach out here.




